These tiny parasites may be crawling on your skin right now
Key Takeaways
You’re most likely carrying a few itty-bitty stowaways and you probably don’t even know it. Say hello to your friendly, bodily parasites! They’re a reminder that even when you’re alone, you’re never truly alone.
Three types of parasites cause pathology in humans: protozoa, helminths, and ectoparasites.
Protozoa are single-celled organisms that can either be free-living or parasitic and are usually spread via a fecal-oral route, as well as by bites from arthropods (eg, mosquitoes or sand flies).
Helminths are also free-living or parasitic and are visible to the human eye, such as tapeworms and flukes.
Ectoparasites include ticks, fleas, lice, and mites, which either attach or burrow into the skin.
You might want to get to know these five parasites, which could be feeding off you right now.
Demodex mite

The Demodex mite is an ectoparasite that lives in or near pilosebaceous units (eg, hair shafts/hair follicles). At lower concentrations, Demodex infestation is asymptomatic, and only pathogenic at high densities or in those who are immunocompromised, thus leading to demodicosis, which may resemble dermatoses.
Two species of this mite are found on human skin: Demodex folliculorum and Demodex brevis. The frequency of infestation in healthy adults varies between 23% and 100%. These mites are invisible to the human eye, with adult D. folliculorum mites between 0.3 mm and 0.4 mm in length and D. brevis between 0.15 mm and 0.2 mm in length. They have eight segmented legs and move at night, remaining ensconced in the hair follicle in the light of day. They feed on skin cells, hormones, and sebum in hair follicles.
Demodex mites are found on eyebrows, eyelashes, chin, nose, cheeks, temples, forehead, balding scalp, ears, and neck, as well as in other seborrheic regions including the nasolabial folds, chest, back, penis, mons veneris, and buttocks—even inside the mouth (in ectopic sebaceous glands in the buccal mucosa).
According to the authors of a review article published in the Indian Journal of Dermatology, “Demodex may act as a vector of transmission of various infections from one area of body to another or between individuals by its potential to ingest and transport various microorganisms that are found in its niche, as demonstrated by potassium hydroxide mount of skin scraping from a mycotic plaque, which showed numerous Demodex mites containing spores of Microsporum canis inside them.”
One potential silver lining to these parasites: Follicle mites harbor immune reactive lipase, which can produce free fatty acids from sebum triglycerides that may defend human skin against Staphylococcus aureus and Streptococcus pyogenes.
Although a limited density of Demodex is non-pathogenic, it may be a good idea to cleanse the face twice daily to keep populations in check. Use non-soap cleansers, avoid oil-based cleansers or greasy make-up, and exfoliate on occasion. In pathogenic cases, Demodex may be eradicated with topical insecticides like crotamiton cream, permethrin cream, and topical/systemic metronidazole.
Lice

Lice are ectoparasites that feed on blood. Three types of lice affect humans: head lice (Pediculus humanus capitis, pictured at left), crab lice (Pthirus pubis), and body lice (Pediculus humanus). Head lice (the most common in humans) are about 2.1 mm to 3.3 mm long, body lice are 2.3 mm to 3.6 mm long, and pubic lice are the shortest at 1.1 mm to 1.8 mm in length.
Transmission of lice requires close contact, as lice cannot jump or fly. Lice can be transmitted by direct body contact (ie, head-to-head) or through fomites, such as headgear or movie seats. In the United States, an estimated 6-12 million people catch head lice, with outbreaks most common in children aged 3-12 years. Girls are affected more commonly than boys.
Pruritis secondary to immune-mediated hypersensitivity may take between 2 and 6 weeks to present, with subsequent episodes of pruritus occurring 1 or 2 days post-exposure. Itching and scratching can lead to bacterial infections, including pyoderma and impetigo.
Historically, lice have been eradicated by hand, shaving the affected area, or using a comb, although cure rates by comb vary widely. Currently, first-line treatment of lice includes lindane, benzyl alcohol, pyrethroids, malathion, topical ivermectin, and spinosad. Ivermectin is the only available oral agent used to treat lice, and although it has proven effective in clinical trials, it’s not FDA approved for pediculosis and can result in neurotoxicity. Nevertheless, it may be an effective second-line therapy for lice resistant to topical therapies.
Public lice are usually treated with the same topical agents used to treat head lice. The treatment of body lice requires good hygiene and proper laundering with the application of insecticide. Infested fomites need to be heat treated to destroy lice and nits.
“Head lice infestation can lead to mental strain and distress in patients as popular media portray affected individuals as unclean,” wrote authors of a review article published in StatPearls.
“Lice have existed for thousands of years, and pediculosis remains a prevalent disease. Treatment failure is common and usually due to inappropriate treatment, lack of compliance, failure to remove live nits, sharing personal care products, failure to treat close contacts, resistance to the drug and failure to clean up the environment,” they added.
Scabies

Scabies is a pruritic skin condition, which is caused by Sarcoptes scabiei, a microscopic mite. Scabies spreads in crowded conditions where people are in skin-to-skin contact, such as daycare centers, hospitals, and nursing homes, as well as between sex partners and family members. Scabies can also spread via fomites such as towels, clothes, and bedding. Notably, scabies is not transmitted from pet to human. (Pets get mange, a different type of mite infestation.)
After initial infestation, it may take 2–6 weeks for symptoms to manifest. In those who’ve been previously infected, symptoms can appear in 1–4 days. Asymptomatic carriers are contagious until all the mites and eggs are destroyed.
Scabies results in a skin rash due to hypersensitivity to mite feces and proteins. Pruritus typically occurs at night, accompanied by a papular rash. Lesions and itching commonly affect the webbing between fingers, as well as wrists, elbows, nipples, waist, armpits, penis, and more.
Scabies infestation sometimes results in tiny burrows due to the female mite tunneling below the skin surface. These grayish-white or skin-colored burrows appear as raised, crooked lines on the skin. Since only 10 to 15 mites typically affect a patient at any one time, these burrows may be hard to detect. Sores from scratching itchy skin can lead to bacterial skin infection, which in turn can lead to post-streptococcal glomerulonephritis.
Crusted scabies is a rare, severe, and massive infestation in people who have an inadequate host response, including the elderly, immunocompromised, or those with disabilities (ie, paralysis) who are unable to scratch. People with crusted scabies are infected with very high numbers of the bugs (up to 2 million!) and are thus very contagious.
The most common scabicide is permethrin cream 5%, but sulfur ointment, lindane lotion, and ivermectin are also used to treat scabies. In addition to treating those infected, all household contacts and sexual partners must be treated at the same time to prevent re-infestation. Fomites, such as clothing and bedsheets, need to be heat treated.
Acanthamoeba
These free-living amoebae are found worldwide in water and soil, and can spread to the eyes via contact lens use, cuts, or wounds. They can also be inhaled via the lungs. Most humans are exposed to Acanthamoeba during the course of a lifetime, but few fall ill.
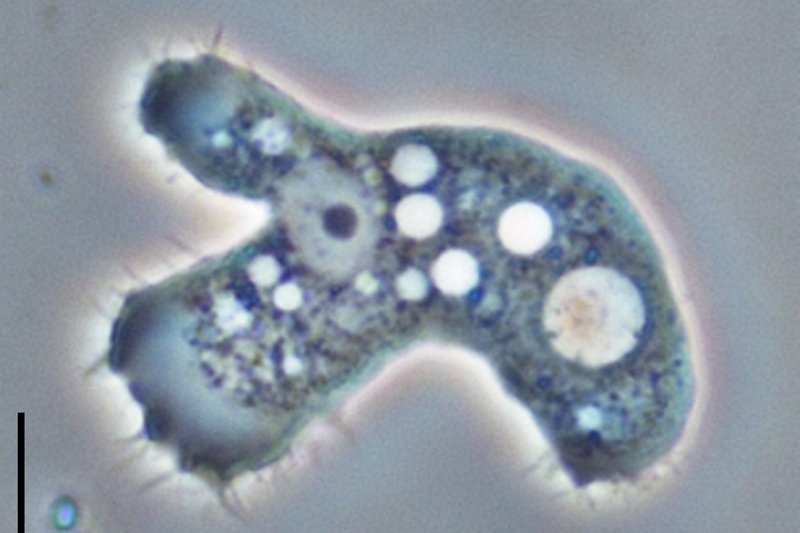
Acanthamoeba have two stages in their life cycle: the infectious trophozoite stage (pictured here) and the dormant cyst stage. (Photo: Jacob Lorenzo-Morales, Naveed A. Khan and Julia Walochnik, CC BY 4.0)
One rare but severe illness that stems from this parasite is Acanthamoeba keratitis, a painful eye infection that can lead to visual impairment or blindness in otherwise healthy people. Two other manifestations—granulomatous amebic encephalitis and disseminated infections—typically occur in those who are immunocompromised.
Early diagnosis of Acanthamoeba keratitis by an ophthalmologist and urgent treatment with prescription eye drops or miltefosine, an orphan drug once very hard to procure, is essential. Even after months of treatment, the patient can be left with a scarred cornea and severe visual impairment.
Chiggers

Chiggers go by many names: harvest mites, red bugs, scrub bites, and bête rouge. These bugs are part of the mite family called Trombiculidae, and are found worldwide, although only two species affect North Americans.
Chiggers only bite when they are larvae, which are almost invisible to the human eye, measuring 0.15–0.25 mm. Chiggers are found on low-lying plants near tall grassy wooded areas or in the vicinity of water. They attach to clothing first and then hop onto human skin at the level of the lower legs, ankles, waistline, groin, axillae, and behind the knees.
Chiggers don’t burrow but rather latch on and secrete an enzyme that dissolves skin and facilitates feeding. Symptoms begin 1–3 hours after a bite, and the digestive enzyme they secrete causes intense itching, which lasts 24–48 hours. Dermatitis resulting from chigger bites presents as an erythematous flat or raised lesion that’s dotted with vesicles or pustules. It can take up to 2 weeks for the rash to resolve.
Chigger bites can be prevented with protective clothing—wearing long sleeves, pants, thick socks, and boots—as well as mosquito repellant. Treatment for the bites is symptomatic with corticosteroid cream and antihistamines employed for relief.