Doctors on edge as practice revenues plunge, survey finds
Key Takeaways
Most physicians have seen a major drop in patient visits because of COVID-19–related stay-at-home requirements. As a result, it’s had a significant impact on their revenues, according to a new MDLinx survey. So, what’s a doc to do? While some have increased their telemedicine visits, it still raises the question: Will this revenue be enough to mitigate the financial losses linked to the pandemic? Short answer, it depends.
“My patient visits went from 35-40 a day to under 10 because of coronavirus. But, if I didn’t do telemedicine, I would be completely shut down right now,” replied a Nevada family medicine physician in response to our survey.
The MDLinx survey was sent out to US physicians by email to investigate the pandemic’s economic impact on their practices; 670 physicians responded. Roughly one-third of respondents are in primary care (family medicine, internal medicine, pediatrics), and the rest are specialists of all stripes (anesthesiologists, cardiologists, oncologists, OB/GYNs, psychiatrists, surgeons, etc).
Nearly 60% of survey respondents are in private practice, including those in solo practice (28%), group practice (23%), and multispecialty practice (8%). About 14% of all respondents work in a hospital-owned practice, 13% work in a hospital setting, and less than 2% are in urgent-care clinics.
Fewer visits
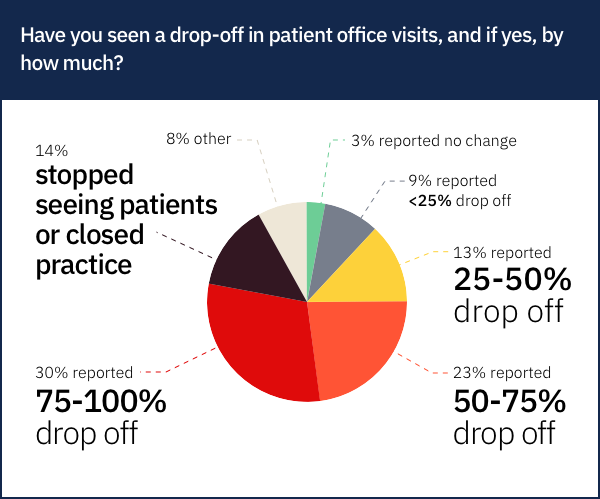
Two-thirds of physicians surveyed say that patient visits have dropped by 50% or more in their practices. This includes about one-third of physicians who report that they’ve lost more than 75% of all their in-person patient visits.
Indeed, nearly 14% of physicians surveyed say that they’ve stopped seeing patients altogether or have closed their practices.
About 13% of respondents say patient visits have dropped 25% to 50%, while 9% report a decrease in visits of 25% or less.
Lastly, only about 3% say they’ve experienced no change in patient visits. (Then again, some of these doctors—anesthesiologists, for example—acknowledge that they don’t have regular patient visits per se.)
With the loss of patient visits, many physicians are turning to alternative avenues to make up for the inevitable loss of revenue. (But, as you’ll see, these might not be enough to make up for financial losses.)
Lower revenues
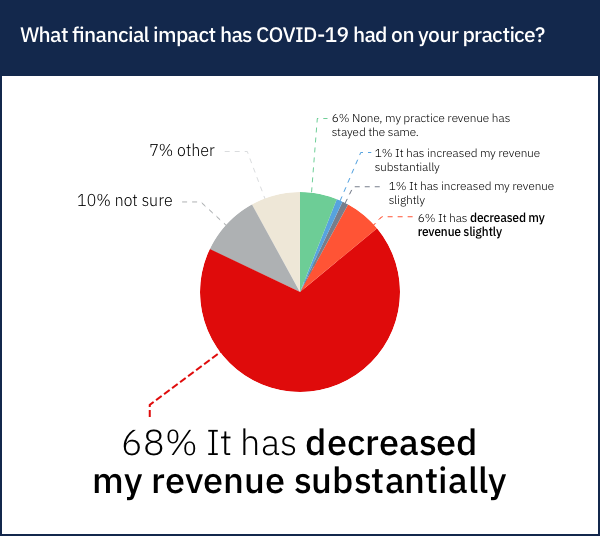
While 6% of physicians report that the coronavirus crisis has “slightly” decreased their revenues, 68% say it has “substantially” decreased their revenues.
“I have no revenue [coming in]. I was offered and have accepted non-paid time off,” said an anesthesiologist at a New Jersey hospital.
While 6% say their revenues have remained the same, nearly 10% aren’t sure yet what effect the pandemic has had on their bottom line.
Only about 2% combined say that their revenues have gone up either slightly or substantially.
As stay-at-home orders and social distancing continue, some practices’ dwindling revenues will run out. And when revenue dries up, cutbacks usually follow. In the current situation, that means laying off staff.
Staff layoffs
With most practices now seeing fewer patients, the most practical cutback is staff. Among our respondents, 32% say their practice/facility has had to lay off staff. Another 32% haven’t laid off staff yet, but they anticipate they may have to.
Nearly 11% have taken other measures, such as decreasing pay, cutting back hours, or putting staff on furlough. “[I’ve] been paying staff as full time out of savings,” said a beneficent Illinois ophthalmologist in solo practice.
Only 26% of physicians said they haven’t laid off staff.
However, many physicians have turned to telemedicine to help keep the lights on and to keep staff on the payroll. But, is it enough to stay afloat?
Increased telemedicine
Social distancing has compelled the general public to take up video chatting through apps like FaceTime and Zoom. Likewise, many physicians have increased their use of telemedicine to keep appointments with their patients.
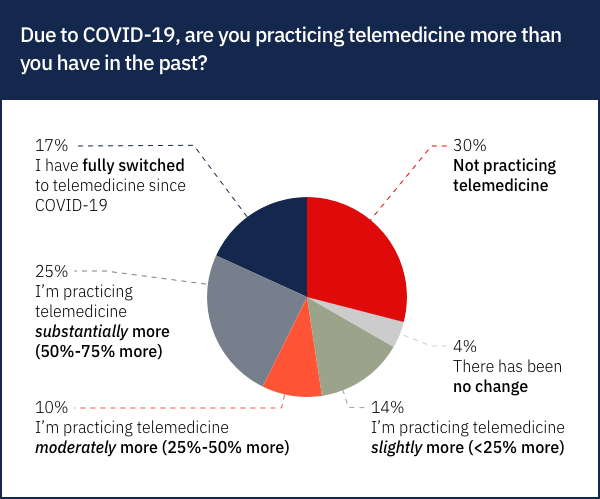
According to our survey, nearly two-thirds of physicians are now using telemedicine more than they did before the COVID-19 pandemic. This number includes about 14% who say they’re using telemedicine slightly more (< 25% more), about 10% who are using it moderately more (25% to 50% more), 25% using it substantially more (50% to 75% more), and about 17% who’ve switched to telemedicine entirely due to COVID-19.
Meanwhile, only about 4% of physicians say they use telemedicine just as much as they did before.
But, about 30% say they’re not using telemedicine at all.
“Gynecology does not lend itself to much telemedicine,” observed an OB/GYN in California. “As a private practice provider who takes insurance, my reimbursement is limited, and it will be difficult to catch up once we can see patients again.”
For many physicians, though, telemedicine has offered a lifeline. It’s a surprising development, since telemedicine has long been waiting in the wings. But now, it has taken center stage. That’s not to say that it’s the financial solution to all practices’ problems, though.
Is telemedicine paying off?
The good news is that physicians can now get paid for most telemedicine visits. With stay-at-home orders in place, the Centers for Medicare & Medicaid Services (CMS) has temporarily expanded coverage for Medicare telehealth services provided to patients nationwide. For the time being, the CMS says it’s considering telehealth visits to be the same as in-person visits, so they’ll be paid at the same rate as regular in-person visits. To make the process even easier, the CMS is allowing physicians to reduce or waive cost-sharing for telehealth visits. Private insurance carriers are expected to follow the CMS’ lead, and some already have.
The bad news? For many practices’ financial solvency, telehealth visits are merely a tiny Band-Aid on a gaping, hemorrhaging wound.
“It is better than no visits, but not as financially beneficial as our previous office visit scheduling,” said an Ohio gastroenterologist in a hospital-owned practice.
Other physicians echoed this sentiment. “Telemedicine is new for us. But, the couple of telemedicine patients we see a day cannot replace the patients we used to see in person. There’s been a 90% drop in business overall,” lamented a California otolaryngologist in a private specialty group.
More than one-third of physicians say that telemedicine has decreased their revenue, either slightly (11%) or substantially (25%). Nearly 10% say that providing telemedicine has had no effect—their practice revenue has remained unchanged.
However, telemedicine has been beneficial for some doctors. In our survey, 17% of physicians report that their revenues have increased slightly, and 2% say revenues have risen substantially.
“I am hoping it will help stabilize the setback,” said a Rhode Island pediatrician in a multispecialty group practice.
Finally, about 1 in 4 physicians just aren’t sure yet whether telemedicine is paying off. “It is too soon to calculate any revenue change,” said a family medicine physician in a solo Texas practice. “Given the lag time in payment from insurance, it will take another month to fully evaluate any changes.”
But, doctors can’t wait any longer. They need financial help right now. Will the federal government provide the solution? For telemedicine, at least, some doctors have this advice for the government:
“Increase reimbursements for telemedicine.”
“Make sure insurers actually pay for telemedicine visits.”
“Provide coverage for phone visits, not only telemedicine visits.”
But, what else can the government do to help struggling medical practices?
Doctors need a bailout
Americans nationwide are praising healthcare workers—not only doctors, but also nurses, assistants, and hospital custodians—for their tireless efforts during this ongoing medical crisis. Should the US government show doctors some love, too? We asked respondents if they believe the government should provide financial help to physician practices. An overwhelming majority (82%) said yes.
As of early April, physicians in private practice can take advantage of small-business relief through the Coronavirus Aid, Relief, and Economic Security (CARES) Act. This act established several new temporary programs to help businesses during the COVID-19 outbreak, including the Paycheck Protection Program, Economic Injury Disaster Loans and Emergency Grants, Express Bridge Loans, and Small Business Debt Relief.
But these programs have been flooded with applications. The Paycheck Protection Program, in particular, has already run out of money and isn’t processing any more applications. The Economic Injury Disaster Loans program is also running out of funds.
So, although many respondents indicated that the CARES Act is a good start, they say there’s more the government can do to help physicians. Here are some of their suggestions:
“Provide rent and other fixed-cost relief.”
“Help with payroll so that we can keep all employees during this difficult time.”
“Provide enough PPE for us to see patients safely.”
“Give physicians hazard pay.”
“Provide 0% interest loans and increase RVUs across the board.”
“Suspend malpractice payments.”
“Provide cost-based reimbursement during this time.”
“Leverage solo practices to perform testing. Give them PPE and incentives to provide coverage, so hospitals are not crowded.”
“Clear med school debt and subsidize those serving high-impact areas.”
“Make sure that hospitals are reasonably compensated for all the care they are giving.”
“Allow physicians to be exempt from taxes for the first quarter.”
“Just allow me to do elective cases as long as I am not using up PPE.”
“Stop questioning testing! In the midst of COVID-19, Medicare is withholding payments for testing performed. Unconscionable! Are they trying to put us out of business while we try to care for people during a very difficult time?”
For now, physicians—already in a financial squeeze before the COVID-19 crisis—must still soldier on, whether or not their pleas and prayers are heard. It begs the question: What will tomorrow look like?
Worries go up to 10
While experts forecast how the coronavirus will continue to ravage both the populace and the economy, no one is truly certain what will happen next. Uncertainty spawns fear. Accordingly, we asked physicians how worried they feel about the future of their practice in light of COVID-19. Physicians graded their level of worry on a scale of 0 to 10, with 0 being the least worried and 10 being the most worried.
The greatest number of physicians chose 5—halfway between being completely worried and being completely unworried. Physicians’ second-most popular choice was 10, the most worried.
“We’re not making enough to cover overhead,” said a frazzled private-practice pediatrician in Alabama. “Can’t do this for long, or we’ll have to close shop.”
How many practices will close? Will telemedicine help practitioners tide things over, or will government programs allow practices to stay in business until they can open their doors to patients again? It’s impossible to say. As has been the case with this historic crisis so far, we’ll just have to buckle up tight and see what comes next.
More Best of 2020:
See all of our best articles, blog posts and journal summaries from the first half of the year.